Emergency room patients whose doctors consult their records through a health information exchange were 30% less likely to be admitted, says a Cornell study.
Emergency department physicians are less likely to admit patients to the hospital unnecessarily when they make use of a consolidated medical record, researchers found in a study published Wednesday in Applied Clinical Informatics.
The study shows that the significant investments New York State has made in health information exchanges (HIEs) at the regional level does, in fact, benefit patients by providing doctors and other healthcare professionals with immediate access to patient records, said Dr. Joshua Vest, an assistant professor at Weill Cornell Medical College and the lead author on the study.
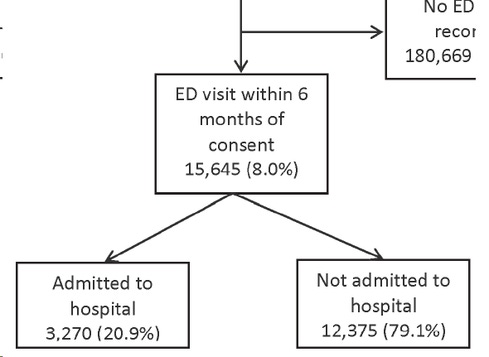
After statistical corrections for the conditions of different patients, the study found that the odds of admission were 30% lower when doctors consulted records from a regional HIE, and that the associated savings equated to $357,000. This was based on a review of claims data for 15,645 New York adults who had an emergency room visit within a six-month period and who had consented to participate in a regional HIE -- specifically, the Rochester Regional Health Information Organization.
[What's after health information exchanges? Read The Quest For Population Health Management.]
Even though all the patients in the study had records available through the HIE, the system was consulted during just 2.4% of those visits. However, those were the visits that had a significantly lower rate of admissions. "Yes, the level of usage was not very high, but it was consistent with what other exchanges see," Vest said. The point is that, "when it was used, it had a beneficial effect on utilization."
Typically, doctors may consult an HIE at their own discretion. When they do not, it can be out of reluctance to use the technology, but not always, Vest said. "For some patients, there is clearly no need. If someone presents with a broken arm, it's a broken arm -- that wouldn't indicate a need to look up all the lab values, look up the history."
When doctors do use the system, they typically are looking for background on a more complicated case in which they have a theory about treatment that prior lab results and medical history might help support. In the absence of access to that information, they might be more likely to order a patient admitted for tests -- even though the same tests might have been performed in the past at another facility -- or otherwise settle on an admission as the more conservative course of action.
Emergency departments don't have access to all historical labs, so without an HIE, it would be too difficult and time consuming to get better information to support or refute a treatment hypothesis, Vest said. HIE data doesn't help doctors make decisions as much as it provides them with data to support their decisions.
The study supports the proposition that community-based HIEs are valuable at a time when many are struggling financially as federal support dries up. Many hospital technology leaders are putting more emphasis on developing their own private HIEs for data exchange. Vest said he has not specifically compared public with private HIEs, though that might be an avenue for future research.
Other academic studies have cast doubt on the value of community HIEs, but Vest said one explanation for the discrepency is that his research focuses on actual use of HIEs, rather than institutional adoption. The organization's endorsement of the technology, while important, "is frequently independent of the acceptance or usage of individuals within the organization."
In addition to influencing hospital administrators and government policy makers, perhaps the study will show doctors that the technology is worth utilizing, Vest said.
Download Healthcare IT in the Obamacare Era, the InformationWeek Healthcare digital issue on the impact of new laws and regulations. Modern technology created the opportunity to restructure the healthcare industry around accountable care organizations, but IT priorities are also being driven by the shift.
About the Author(s)
You May Also Like







