Both payers and providers support a shift to value-based payments, a study says.

20 Tests Healthcare CIOs Must Juggle
20 Tests Healthcare CIOs Must Juggle (Click image for larger view and slideshow.)
Healthcare's familiar fee-based payment model is rapidly disappearing.
By 2020, two-thirds of payments will be based on value measurements, up from one-third today, according to The 2014 State of Value-Based Reimbursement (registration required), published Wednesday. The study, commissioned by McKesson and conducted by ORC International, was published at this week's AHIP Institute 2014 conference.
Both payers and providers want healthcare to move away from fee-based payments, the study found. Today, 90% of payers and 81% of hospitals provide a blend of fee-for-service and other reimbursement models, according to the report. Payers expect fee-for-service to decrease to 32% in five years from 56% today. Hospitals that use a mixed approach today expect similar results: 34% project fee-for-service use in five years, compared with 57% in 2014.
"The most striking thing is how aligned the payers and providers are about both where they are today and where they see things going," Dr. David Nace, vice president and medical director at McKesson Health Solutions, said in an interview. "It's heartwarming because what's needed is alignment."
[Can technology help healthcare adapt to a changing payment structure? Read Healthcare's Big Challenge: How To Measure Value.]
It's particularly striking considering that 60% of payers believe value-based reimbursement will improve profitability, but only 35% of providers share that view, according to the study. Indeed, smaller providers are even more leery: 29% think value-based models will improve their financial state, compared to 40% of larger providers. However, those that participate in an Accountable Care Organization (ACO) are more optimistic about the outcome.
Perhaps because of this expectation, ACOs are leading the charge to value-based reimbursement -- and 45% of hospitals already participate in an ACO, according to the study. However, Dana Benini, vice president of ORC International, pointed out in an interview that another 59% expect to join an ACO by 2020. The number of ACOs has tripled in two years.
Likewise, regional differences impact organizations' readiness. Collaborative areas of the United States -- regions with one or two players and hospitals that clearly lead their area -- are often closer to value-based reimbursement, the report found. Regions with multiple players and fragmented leaders are more likely to continue using fee-based payments.
"Each customer's taking a different approach, depending on their region and the dynamics of their hospital systems, the strength of their payers," Carolyn Wukitch, senior vice president and general manager of network and financial management at McKesson Health Solutions, said in an interview.
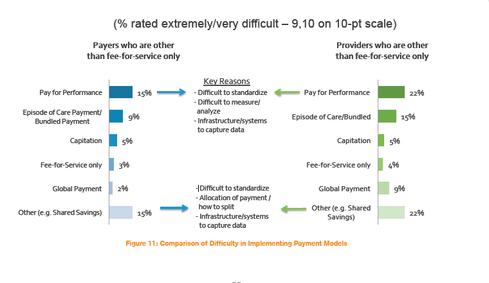
Despite a desire to implement pay-for-performance (P4P), both payers (15%) and hospitals (22%) find this measure extremely difficult or very difficult to implement. In addition, 9% of payers and 15% of hospitals said episode of care/bundled payments were very difficult or extremely difficult. Both parties cite a lack of standards, analysis tools, and a need for better IT infrastructure and systems before they can implement P4P.
In fact, technology lies behind all key obstacles for payers and providers. Forty-one percent of payers and 23% of hospitals cited their need to integrate internal, vendor, and collaborative IT systems; 22% of payers and 20% of hospitals pointed to data collection, access, and analytics requirements. In order to generate clinician buy-in and engagement for value-based reimbursement, 20% of payers and 17% of hospitals once again turn to technology as the key catalyst, the study found.
"Training the trainer is critical," said Nace. "This is a complex world. It's not 'pull a switch and move from one to the other.' Even within a health system or payer, this is culture change. You really need to make a concerted effort. The systems are in place. Lots of pilots have been done. We're now in a good place, all the parties, to make this scalable and put it into action."
Download Healthcare IT In The Obamacare Era, the InformationWeek Healthcare digital issue on changes driven by regulation. Modern technology created the opportunity to restructure the healthcare industry around accountable care organizations, but ACOs also put new demands on IT.
About the Author(s)
You May Also Like