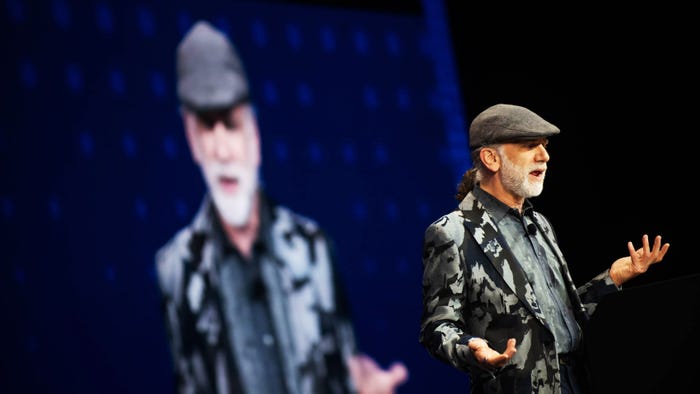
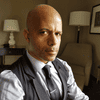
Paul Nakasone, former director of the National Security Agency, and a former commander of US Cyber Command, speaks at the RSA Conference 2024.
Cyber Resilience
Four Horsemen of Cyber Reunite at the RSA ConferenceFour Horsemen of Cyber Reunite at the RSA Conference
Paul Nakasone. Timothy White. Stephen Davis. Jen Easterly. The quartet who drafted plans for US Cyber Command discussed their shared history in cyber defense.
Never Miss a Beat: Get a snapshot of the issues affecting the IT industry straight to your inbox.


















.jpg?width=300&auto=webp&quality=80&disable=upscale)