Medicine: Will The Tech Bubble Break?
How do we translate the froth of healthcare technologies into better healthcare?
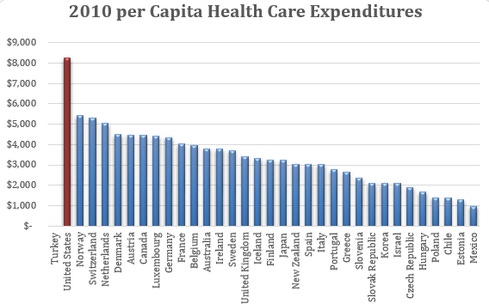
We here in the United States enjoy the most expensive medical care (or is that disease care?) in the world, yet rank towards the bottom of many health measures of the Economic Cooperation and Development (OECD) nations.
I’m fond of pointing out that "everything is connected to everything." Proposed solutions often have unintended consequences that may be worse than the problems they were meant to solve. We can see elements of this in the troubled rollout of the Affordable Care Act and piecemeal attempts to control the unforeseen consequences of well-meaning regulations seemingly gone awry. It’s almost certain there will be other short-term “fixes” that will be announced that will lead to further entanglements requiring more fixes.

Source: Barbara Starfield, MD, MPH. JAMA July 26, 2000
Everyone is clamoring that we need our healthcare system to be more affordable and deliver more value. Our healthcare system has gotten so massive and woven into the fabric of our economy. According to the OECD in 2012, more than 19 million people are employed in health and social services (a little over 13% of the work force) of whom almost 50% are in supportive and administrative roles (Bureau of Labor Statistics). I’m not sure those trying to cut healthcare costs have really thought through the economic impact their proposed cuts will have. Healthcare has been one of the bright spots in our economic recovery.

Source: Peter G. Peterson Foundation
In this respect, healthcare spending is similar to military spending. Do we really need to spend more than the countries of China, Russia, UK, Japan, France, Saudi Arabia, India, Germany, Italy, and Brazil combined? But when cuts are imposed, as in the recent sequester, the impact of lost local jobs is so painful it’s politically and economically untenable. We are more dependent on military spending and healthcare care spending than we are willing to admit.
[What should change in 2014? Healthcare Tech Leaders Share New Year's Resolutions.]
Technology has been touted as a tool that will help reduce costs. We have seen many industries leverage technology to dramatically improve productivity, reduce the human capital needed to produce products, and increase profits. But, as Steven Brill in his seminal Time magazine article pointed out, “unlike those of almost any other area we can think of… the advance of technology has made medical care more expensive, not less.” We now employ more people in healthcare than we ever have before, and the growth does parallel the increased use of technology in healthcare.
Isn’t this bad? Or is it good?
It’s been quite apparent to me, as a practicing primary care physician, we spend an inordinate amount of time and resources treating chronic conditions that are in large part the result of lifestyle decisions. We cannot medicalize our way out of this. We also cannot change lifestyles effectively from within jail-cell exam rooms in which we are forced to see patients. We have to get more involved and active in our patients' lives to improve their lifestyles in order to reduce their disease burden.
This is where the impending convergence of big data, mobile technology, and social media may come together to give us the opportunity to lower the cost of disease, while at the same time increasing our spending on health.
We all have demonstrated that we’re willing to spend enormous amounts personally on items we think will improve our health. We Americans spend a staggering $33.9 billion a year on complementary and alternative medicine. We just don’t like spending anything on disease.
In the last decade we’ve experienced a dramatic movement of processing power from the office into our hands. We carry more computing power in our phones than we could have purchased for our offices just a few years ago. For example it is now possible to use smartphone cameras to measure, not only our pulses, but even oxygenation and stress levels. Embedded motion sensor chips and coprocessors are broadening the sensing capabilities at a dizzying rate.

Heart Rate Monitor from Azumio
No one doubts that eventually just about every diagnostic device will have a mobile version. Qualcom’s $10 million Tricorder competition to “bring healthcare to the palm of your hand” is just one of many efforts fueling this movement.
When this data is coupled with cloud-based analytic tools like IBM’s Watson and with a person’s social network, we should see medicine freed from its claustrophobic walls and into everyone’s hands to be used at any time.
One of the two organizations for which I work is participating in two at-risk Accountable Care Organizations, and we’re aggressively targeting remote monitoring and “hospital at home” services for the very sick. In an ACO reimbursement model, the small fraction of patients that used to account for so much of our revenues now account for costs that we can’t afford. By taking care of them, we are tasting the potential of a switch in revenue sources from face-to-face to virtual care that has the potential to dwarf previous healthcare business models.
So what will be the value of huge buildings filled with diagnostic devices when they have shrunk, and we physicians and patients carry them? Dr. Michio Kaku, in his book The Future of Physics, describes hand-held MRI devices and predicts that in the near future the majority of medical care will be in the home. What will be the model of care when every person is armed with consumer technologies that do what now takes an army of technicians and physicians to use?
I don’t think we can effectively lower the healthcare burden by administrative brilliance, bureaucratic action, legislative motions, regulatory statutes, or any traditional approaches. We have ample evidence that each of these measures just leads to another layer of complexity and cost. We have to take another approach, and I believe that mobile health will lead the way.
My own prediction and hope is that we in healthcare will seize the opportunity to leverage technology and move away from ridiculously expensive disease care to immensely profitable and valuable healthcare. If we do, the bubble is just beginning to fill. If we don't, then healthcare is the next bubble to burst.
David Voran, MD, is Assistant Professor and Informatics Director of Community and Family Medicine at Truman Medical Center. He is Medical Director of the Innovation Clinic at Platte City for Heartland Health and is a Collaborative Physician for CVS's Minute Clinics in the Kansas City Area.
Healthcare providers must look beyond Meaningful Use regulations and start asking: Is my site as useful as Amazon? Also in the Patient Engagement issue of InformationWeek Healthcare: IT executives need to stay well informed about the strengths and limitations of comparative effectiveness research. (Free registration required.)
About the Author
You May Also Like